Wellbeing is the new buzzword alongside resilience and mindfulness. Many industries are experiencing burnout. In my opinion, all healthcare professionals have probably experienced some form of burnout in the last 2 years, even if they are not aware.
The definition for wellbeing is:
A state of happiness and contentment, with low levels of distress, overall good physical and mental health and outlook, or good quality of life
APA dictionary
Hospitals are ramping up their well-being activities with yoga and mindfulness classes. But I’m here to say, Yoga is not the solution for burnout!
How do you assess burnout?
When I ventured into leadership, I wanted to make a difference by advocating for Advanced Practice Providers (Nurse Practitioners and Physician Assistants) in their role, but I didn’t know where to start. With the support of my physician colleagues, I surveyed my team to assess for burnout and determine the biggest challenges in their role. The results of the survey revealed that 60% of the APPs met the threshold for burnout. How do I manage a team that is burned out? And so began my interest in burnout and wellbeing practices.
Many clinicians and even my previous staff would hear the word wellbeing and would immediately roll their eyes. If I added a wellbeing topic to a meeting agenda, a few would not participate or would say it is a waste of time. My physician colleagues have told me, “Well that’s an individual thing. It’s upon the individual to determine their wellness.” And I agree, well partially. A person should take some accountability in supporting their mental and physical well-being, and their happiness. However, what if they are not able to do so in their work environment?
For example, it would drive me crazy when my team members would say, “No, I can’t eat today. The ED is too busy.” Or I would remember my days in the PICU when we did not use the bathroom the ENTIRE 12-hour shift, and then bladder scan ourselves at the end of the day to determine how much urine we could hold. 😬🤦🏽♀️ Once masks mandates were instituted during the pandemic, do you know how hard it was to remain hydrated in between patients? Or find a place to eat safely, 6 feet away from everyone else? It was near impossible!
Leadership gives you the opportunity to change culture
One of the great things about leadership is that it exposes you to opportunities to make a difference. In my last role, I co-lead the APP enterprise-wide committee to support the 700+ APPs in creating a culture of wellbeing. I worked with an amazing NP (Thanks NL) who taught me so much about advocating for APPs and pushing the boundaries just enough for change to occur. Our work involved assessing APPs for burnout, supporting wellbeing programming for APPs, and collaborating with hospital leaders to implement system changes that would support the workforce and increase their wellbeing. However, the most important part of this work was meeting with various leaders on how we could shift to a culture of wellbeing through minimizing challenges in documentation, scheduling, and increasing psychological safety. The work was exhilarating but challenging!
Recently, the National Academy of Medicine held a webinar entitled “Clinician Retention in the Era of COVID: Uniting the health workforce to optimize wellbeing.” The US Surgeon General, Dr. Vivek Murthy, who is leading this task force told leaders that it’s not just about creating wellbeing programming or suggesting that clinicians do their individual practices but it’s about creating a culture that allows time for patient care, documentation, etc. Hospitals across the nation presented their initiatives and spoke about the importance of having well-being advocates in the C-Suite.
How do nurses promote wellbeing?
Nurse leaders (and even leaders in other industries), the well-being of your team (and yourself) should be a top priority! Think about it, if your staff does not feel supported or well at work, there will be:
Currently, many organizations are beginning this work and creating centers of wellness or wellbeing with the support of their C-Suite. If you are a nurse leader, and these conversations are not occurring at your hospital, you can be the beacon of change. When you meet with your boss, director, or leader discuss why this is important for your institution.
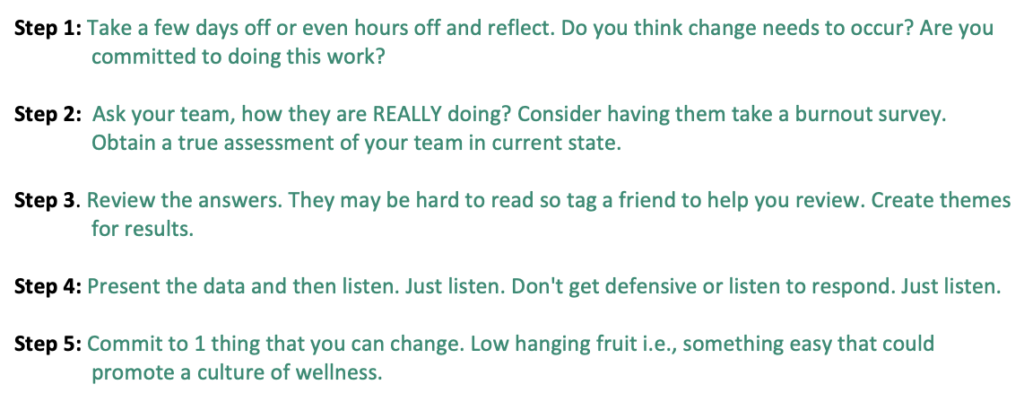
If you want to determine how to start this work within your clinical, here is a starting guide.
To all my fellow nurse leaders who are working tirelessly to maintain the healthcare system, I completely understand this does not seem like a top priority. But it is! If you consider your team’s well-being as part of your decision-making, you will make a difference for your staff, patient care, engagement, and retention. Offering wellbeing practices is helpful as well nurses but it is not the complete answer. As a leader, you can champion this change in your setting. If not you, then who?
Want to hear more, listed to interview on Dr. Tomi Mitchell’s podcast. I love brainstorming about creating cultures of wellbeing in nursing. Let me know your thoughts in the chat or send me a message.


